When Liam Thorp, Political Editor of the Liverpool Echo tweeted on Wednesday that his doctor had mistakenly classed him as morbidly obese by recording his height as being 6.2cm instead of 6ft 2in we all had a good laugh. No harm done! But this simple clerical error at the GP surgery highlights a national issue that runs to the core of why the UK has one of the highest rates of death from COVID-19 in the world and why we are finding it so difficult to remedy the situation. By back-tracking through the obesity figures it seems that 60% of obese people in England might be unfairy excluded from priority vaccinations.
So I’m not getting a vaccine next week – was feeling weird about why I’d been selected ahead of others so rang GP to check. Turns out they had my height as 6.2cm rather than 6 ft 2, giving me a BMI of 28,000 😂
— Liam Thorp 💙 (@LiamThorpECHO) February 17, 2021
While doctors have known for some time that obesity is a contributory cause of many health conditions, the public were less aware of the risks. Obesity in general and unhealthy diet in particular are now considered to be the largest risk, overtaking smoking, principally because fewer people smoke these days. Eating and drinking too much, as well as exercising too little displays what is called a dose response. The fatter* you are the less likely you will be to enjoy a long and healthy old age. But studies have shown that simply reducing your body weight by 5% or 10%, however overweight you are, will have a beneficial effect. The remedy if very different to the remedy for smoking. You don’t have to give anything up, but you do have to make changes. These changes must include eating less and eating better.
A recent study has highlighted all the attendant risks to longevity associated with obesity. The results are shown below;
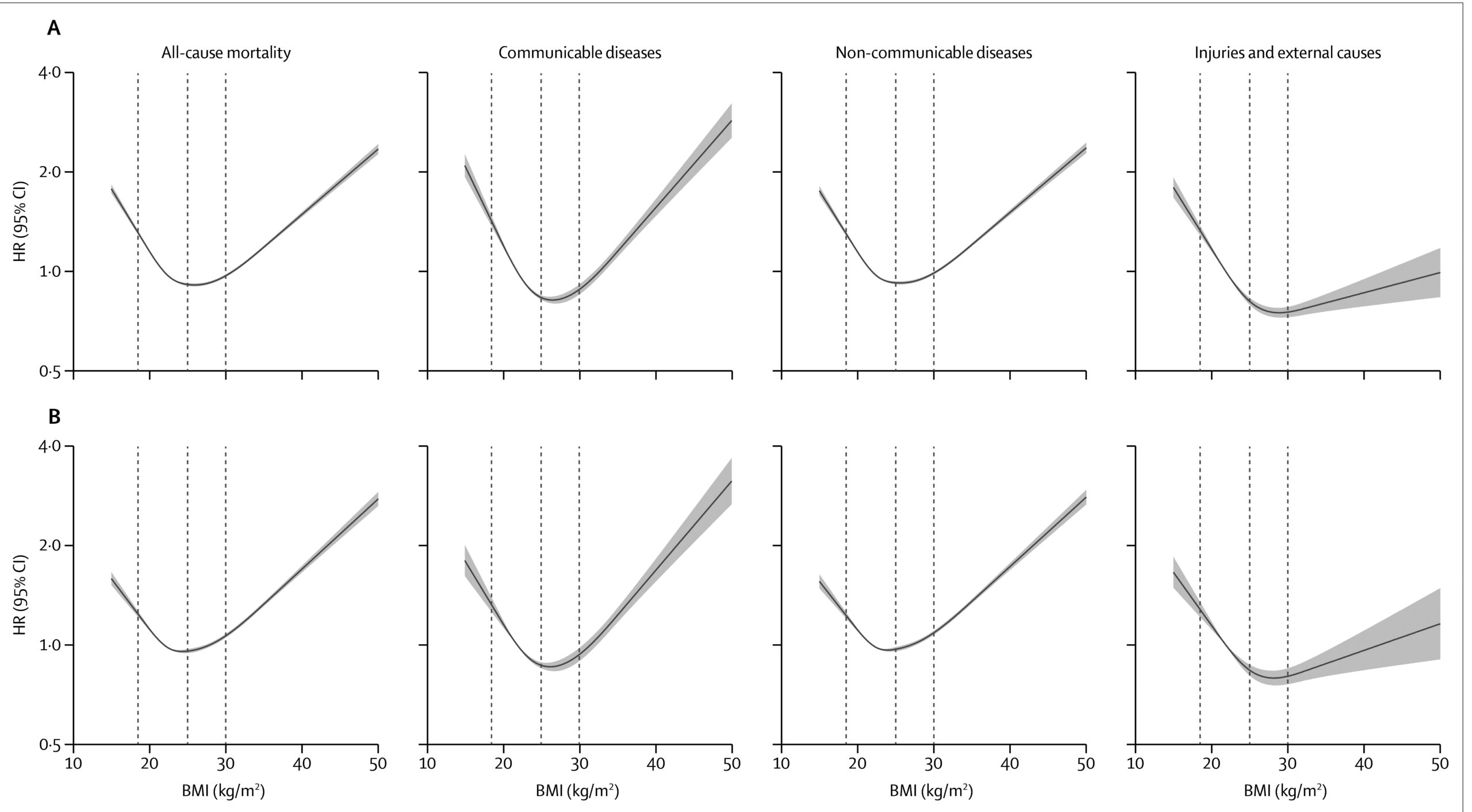
What we see are a series of graphs, all of which show very similar forms, with a short uptick at low weight (below average BMI can be equally dangerous) and a long but not necessarily linear increase above average healthy weight. These shapes are called J shaped curves or hockey stick curves. This study, completed in 2018 confirms the effect among 3.6 million adults in the UK. It is as near as any scientific study gets to irrefutable proof that being overweight can cause increased mortality[i].
COVID-19 has brought into stark relief the fact that suffering from diseases such as cancer, diabetes, heart disease, frailty and dementia all increase the risk of hospitalisation and death. What this study demonstrates is that one of the major risk factors for all these illnesses is being overweight. Doctors have always been aware that diseases such as influenza and pneumonia are often more acute amongst those patients who are already suffering one of these other co-morbidities. Being overweight is not a good place to be.
Liam Thorp had inadvertently stumbled upon a fault in our public health system, that would be amusing if it were restricted to simply one or two case, but seems to deny many people good health care. We have little idea how many of the population are overweight and have no way of contacting those who are. This limits our ability to manage programmes to help the overweight lose weight. At the moment the situation is critical, as this lack of knowledge is limiting the rollout of COVID-19 vaccines to those morbidly obese, but younger people, who are higher risk.
The only obesity data the NHS will have on your situation is gleaned from GP records. However, these records are riddled with inaccuracies. They are often out of date, or simply missing data from people who never visit the surgery. In addition, some GPs find it difficult to ask a patient who is obviously overweight to get on the scales. They cannot force them and even if they have the time to coax them onto the machine, they don’t have the time to fully discuss weight loss with a patient.
The Health Survey for England[i] takes a representative sample of adults aged 16+ (about 8500) and from this data provides estimates of the prevalence of obesity. The 2019 survey, found that 28.0% of adults in England are obese and a further 36.2% are overweight, making a total of 64.2% who are either overweight or obese. However, 30% of those surveyed refused to be weighed, reducing our confidence in even these figures. I’m not able to find the calculated confidence interval in these figures. But I will persevere and update this post when I find it. My guess is that it is very large. To me it seems obvious that those who refuse to be weighed are more likely to be overweight!
This might not matter if our GPs kept copious records for each of us. But a recent House of Commons report noted that cases of adult obesity as recorded by GPs range from 7% to 12% depending of the level of deprivation in a particular area, while they suggest that estimates of the true prevalence across England are 29% [ii]. About 26 million people are under 60 and over 18 in England. So GPs inaccurate records could miss out over 4 million people, who should be prioritised now. The most time strapped doctors, in the poorer regions, have the most obese patients. During the pandemic the level of obesity in this country has contributed to our disastrous record. Let’s hope that during the vaccination process we manage to right that wrong.
* Do not assume that I use the term fat in a pejorative way. It is weight of fat, not weight of muscle that is the problem here, so while body mass index (BMI) is a good rough guide, it is not definitive.
[i] 2 NHS Digital, Health Survey for England, 2019 https://digital.nhs.uk/data-andinformation/publications/statistical/health-survey-for-england
[ii] House of Commons Health inequalities: Income deprivation and north/south divides Insight Guide.
Published Tuesday, 22 January, 2019
Insighthttps://commonslibrary.parliament.uk/health-inequalities-income-deprivation-and-north-south-divides/
[i] Krishnan Bhaskaran et al, 2018. Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3·6 million adults in the UK. The Lancet, Volume 6, Issue 12, p944-953, December 01, 2018. Published:October 30, 2018 DOI:https://doi.org/10.1016/S2213-8587(18)30288-2
This year I shall be maintaining a weekly blog, covering pre-publication excerpts from the book as well as a series of articles about the science and the scientists who have unlocked the secrets of longevity. Please register your interest by clicking on the mailing list below.
A beta reader is a test reader of an unreleased work (similar to beta testing in software), who gives feedback to the author, from the perspective of an average reader. If you’d like to help me get this book as good as it can be, I’d love to hear from you. You’ve got plenty of time to make up your mind. The chapters will be ready from June onwards. I’m sorry there is no fee for this work, except a free copy of the finished book and an acknowledgement. This is not a commercial exercise. Say Tomato, the publisher of the book and of the website is run as a self-financed social enterprise. I shall be eternally grateful. Any profits from Glorious Summer will be directed into Say Tomato’s work for women over 40.
Contact me directly wendy@wendyshillam.co.uk if you are interested, giving a brief description of yourself and your reading experience. (It doesn’t matter if you haven’t done any beta reading before – avid readers make the best beta readers.) Thank you.

Wendy Shillam
Trained in environmental and bio-sciences, Wendy Shillam is a registered clinical nutritionist, specialising in longevity. She is the founder of the social enterprise Say Tomato! that provides free and trusted weight loss advice for women over forty. This part of the blog is a precursor to publication of her book, Glorious Summer – the secrets of longevity. You can read about it here.

Again Wendy, very interesting reading. We ever seem to be finding fresh ways to endanger ourselves by the way we live, whether this can be termed deliberate, as in taking up a habit like smoking that is widely known to be harmful, or a consequence of a poor dietary regime from childhood. There is a deep and abiding disconnect among us in that we lament the tragedy but cannot overcome the behaviour that results in it. On the same news schedule we hear of a looming mass famine in Yemen and a successful landing on Mars. Who would have thought space exploration an easier objective than feeding people? We are undoubtedly more sophisticated than our forebears but hardly any wiser it seems.
Thanks Alex,
We cannot necessarily always choose how we eat or what our state of health has been. This is what Quetelet was saying a hundred and fifty years ago Genetics, environment and life all get in the way! But whatever category we are in, we can always get help and advice to help us improve our lot.